Billing via Availity
Availity will only accept Claims for the Payers listed: https://apps.availity.com/public-web/payerlist-ui/payerlist-ui/
This assumes you already followed the steps on how to generate the 837P from Office Puzzle described here: https://www.officepuzzle.com/tutorials/billing/
How to Upload a File in the Availity Portal
1. Log in to the Availity portal.
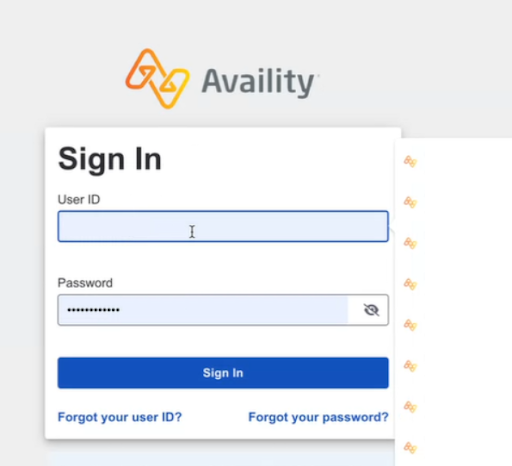
2. Click on Claims & Payments, then select Send and Receive EDI Files.

3. Select the organization name and click Submit.
4. On the Send and Receive Files page, click the folder Send Files.
5. Choose the file you want to upload and click Submit to send it to Availity.
6. Check the receive files folder for Availity’s response
If you have any questions or issues during the process, check the batch status and ensure that you have followed each step correctly. 🚀
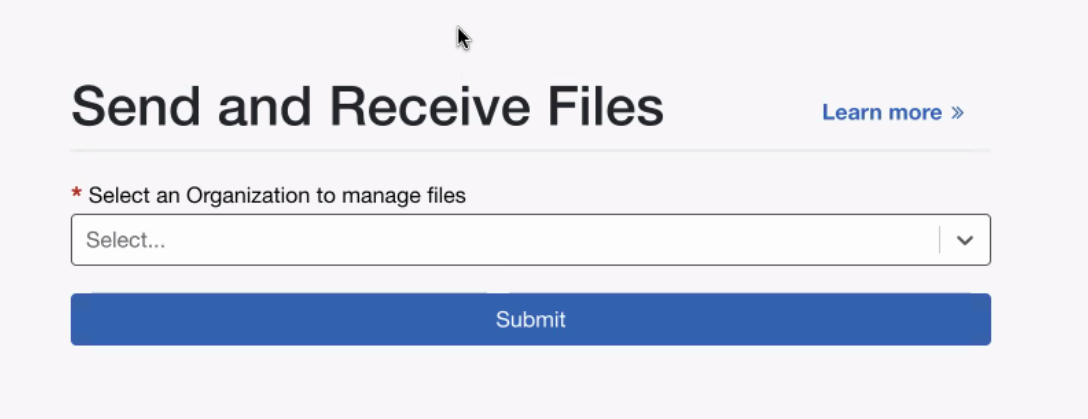
Billing via Sunshine Health (Centene)
Sunshine Health Portal (https://provider.sunshinehealth.com/careconnect/login/oauth2/code/pingcloud&brand=sunshinehealth) will only accept Claims for the following payers: CMS Title 21, CMS Title 19 and Ambetter.
How to Submit a Batch to the Sunshine Portal
Follow these steps to successfully upload a batch to the Sunshine Health portal.
1. Go to the Sunshine portal using the following link: 👉 Sunshine Health Portal.
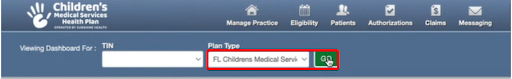
2. Select the corresponding Plan Type and click Go Button.
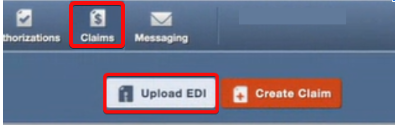
3. Navigate to the menu and click Claims → Upload EDI.
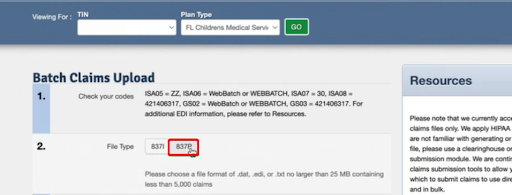
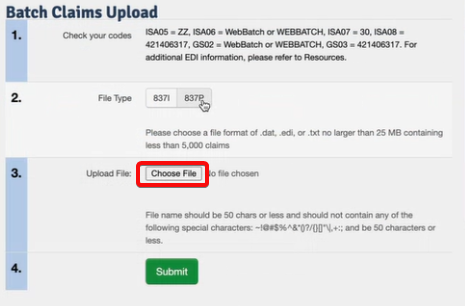
4. In the new window titled Batch Claims Upload, go to Step 2 and select the option 837P.
5. Click Choose File and select the file you previously downloaded from Office Puzzle.
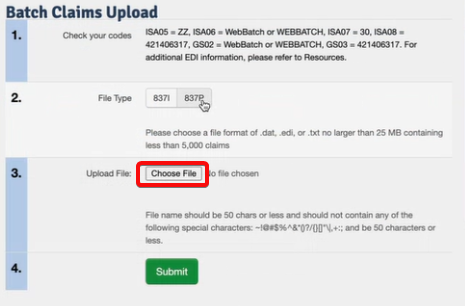
6. Finally, click the Submit button to upload the file.
How to Verify That the Batch Was Uploaded Successfully
After uploading the batch, it is important to check that the system has received it correctly.
1. In the menu, click Claims → Batch.
2. Filter by the date you uploaded the batch and click Search.
3. The system will display a list of submitted batches:
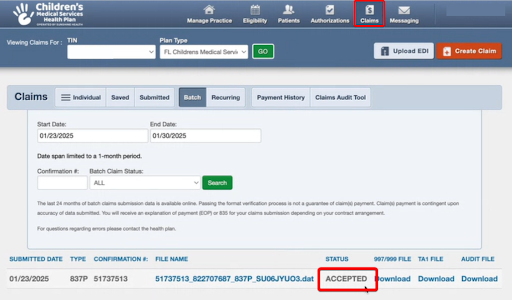
Accepted: The batch was received successfully.
Rejected: There was an error, and the batch was not accepted.
How to Check the Status of Each Claim
If you want to verify the individual status of each claim submitted, follow these steps:
1. In the menu, click Claims → Individual.
2. Filter by the date you need to check and click Search.
3. The system will display a list with the following details: client, billed amount, claim status
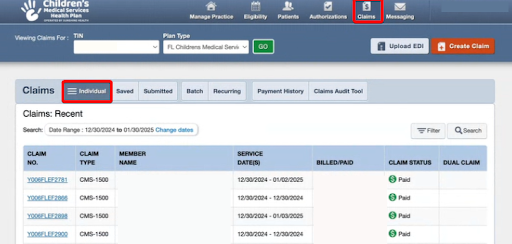
Paid: The claim has been paid.
Process: The claim is still being processed.
✅ Done!
By following these steps, you can successfully submit and verify your batches in the Sunshine Health portal. 😊
If you have any questions or issues during the process, check the batch status and ensure that you have followed each step correctly. 🚀
Billing via Claim.MD
Please remember Claim.MD is offering 20% discount to all accounts using Office Puzzle as their EMR. Simply mention this during registration or send a ticket requesting the discount.
Claim.MD will only accept Claims for the Payers listed: https://www.claim.md/payer-list
This assumes you already followed the steps on how to generate the 837P from Office Puzzle described here: https://www.officepuzzle.com/tutorials/billing/
Payer Enrollment
This is the process where we make sure Claim.MD is aware of which payers we are sending to, this also ensures we configure the ERA (Electronic Remittance Advice) to receive the payments once the claims are processed. Although this step is NOT mandatory is highly recommended.
1. Go to the Claim MD portal https://www.claim.md
![]()
2. Enter your Claim.MD username and password to log in.

3. In the menu, go to Provider Enrollment.

4. In this section, locate the payers and click the Enrollment Required button.
5. Follow the provided instructions to complete the registration for each payer. This requires for you to register your Group NPI with Claim.MD for each payer.
6. Once all payers have been registered, you can proceed with the batch upload.
Note: The registration process may take some time to be completed. Make sure to check the status of each payer before proceeding.
Manually Uploading Claims
Uploading Files Manually
"Manually Uploading Claims" refers to the process of generating a batch file containing all claims for a specific provider from the Practice Management System or other software system. This file is typically in ANSI X12 format, although it may be in other formats such as PDF, CSV, XML, or others. The batch file is then saved in a local drive and uploaded into Claim.MD.
This assumes you already followed the steps on how to generate the 837P from Office Puzzle described here: https://www.officepuzzle.com/tutorials/billing/
To upload a claim:
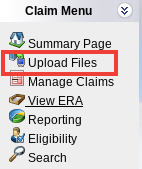
1. Click Upload Files on the left-hand navigation menu.
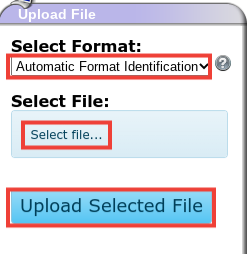
2. It is recommended to leave Select Format dropdown as Automatic Format Identification first.If the document is not being automatically read, try selecting the specific format (CSV, XLS, XML etc.) in the dropdown.
3. Click the Select File button
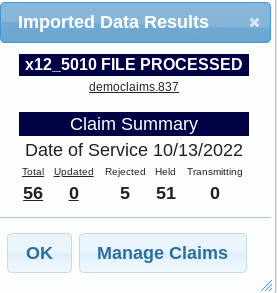
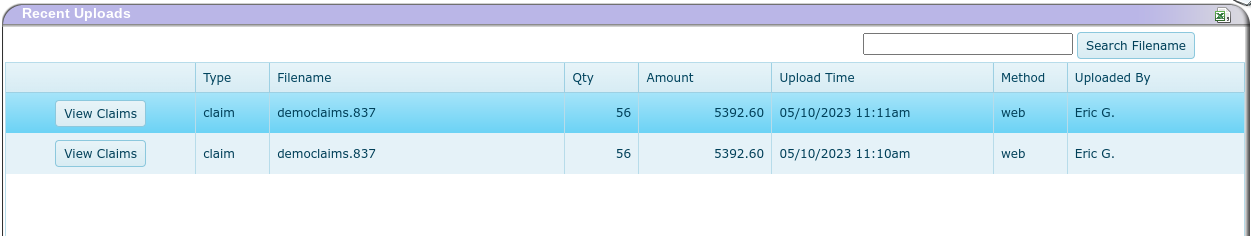
7. The Recent Uploads section of the page is where you can quickly view information about your batch file such as quantity of claims in the file, total amount for the claims, etc.8. Click the View Claims button to see the individual claims in the file.
You can find the original for this tutorial at https://docs.claim.md/docs/uploading-and-entering-claims
Clearing House integration
Name: Clearing House integration within Office Puzzle
Description: How to add a Clearing House to your account in Office Puzzle.
Difficulty: Middle
Duration: Less than 6 minutes
Please check https://www.officepuzzle.com/tutorials/billing/ for a standard billing
Summary:
Step 1- From the Agency Dashboard, access Billing.
Step 2- Click on Batch Claims.
Step 3- Click on +New Batch.
Step 4- Select Payer.
Step 5- Select Health Plan.
Step 6- If the Clearing House for the selected insurance is not configured, the system will prompt you to set it up. Click Yes.
If you already have a configured Clearing House select that integration if not select New Integration.
Step 7- Select the appropriate Clearing House for the payer and complete the required information, a Default Clearing House configuration is typically more than enough.
Step 8- Follow the rest of the steps described at: https://www.officepuzzle.com/tutorials/billing/
Clearing House integration within Office Puzzle
Step 1- From the Agency Dashboard, access Billing.
![]()
Step 2- Click on Batch Claims.
![]()
Step 3- Click on +New Batch.
![]()
Step 4- Select Payer.
![]()
Step 5- Select Health Plan.
![]()
Step 6- If the Clearing House for the selected insurance is not configured, the system will prompt you to set it up. Click Yes.

If you already have a configured Clearing House select that integration if not select New Integration.

Step 7- Select the appropriate Clearing House for the payer/health plan.

Complete the required information, a Default Clearing House configuration is typically more than enough.

Step 8- Follow the rest of the steps described at: https://www.officepuzzle.com/tutorials/billing/