Why Data Collection is Important in ABA Practices
Applied Behavior Analysis (ABA) is a research-based behavior therapy that helps people with autism and developmental disorders increase positive behaviors, decrease negative behaviors, learn new skills, and improve social relationships. Every treatment plan and modification depends on accurate and timely data collection. Without reliable data, ABA practitioners cannot deliver their core promise of evidence-based care.
With 1 in 31 children in the US diagnosed with autism each year, and the demand for BCBAS significantly outpacing the number of licensed practitioners, ABA practices face increasing challenges in serving the growing needs of clients. As the field grows and practices scale, efficient and accurate data collection is critical to delivering quality care, and promoting staff wellbeing and retention.
Read on to learn more about commonly used ABA data collection methods, how and when to use them, and how modern software tools can support ABA staff in providing strong clinical outcomes with less burnout.
Key Takeaways
- Accurate data collection is essential for evidence-based ABA therapy and directly informs treatment decisions, progress monitoring, and accountability.
- ABA data collection methods fall into two main categories: continuous and discontinuous measurement—and choosing the right method depends on behavior type, setting, and clinical goals.
- Digital practice management and data collection software can significantly improve efficiency and accuracy while reducing staff burden.
What Is Data Collection in ABA?
Data collection in ABA is the systematic recording of behavioral and environmental variables to measure change over time. Across the discipline, behaviors are operationally defined so that they can be observed, measured, and replicated consistently by different therapists in various settings. This structured approach allows clinicians to determine an intervention’s effectiveness and whether modifications are needed.
The primary purposes of data collection in ABA include:
- Evaluating intervention effectiveness.
- Tracking behavior change over time.
- Identifying patterns or triggers.
- Adjusting treatment programs.
- Meeting payer, compliance, and ethical requirements.
Data Collection Ethics and Effectiveness
An ethical approach to measurement is crucial for BCBAs and staff within ABA practices. Initially, the client’s values and needs are taken into account when developing measurement goals and the course of treatment. Then, measurement approaches are selected that are aligned with the behavior, setting, and program decisions to ensure the best possible outcomes.
The BACB Ethics Code outlines additional measurement goals and approaches to ensure that practitioners:
- Measure behaviors that impact quality of life, safety, independence, or access to learning.
- Regularly review data to evaluate treatment effectiveness.
- Balance data precision with feasibility to reduce staff fatigue and errors.
- Share data in an understandable format with clients, caregivers, and funders.
- Monitor and maintain interobserver agreement (IOA) when applicable.
Because analysts are responsible for choosing data methods that best align with treatment goals, it is crucial that they understand the strengths and limitations of each measurement method they use.
Main types of Data Collection Methods in ABA practices
ABA data collection methods are divided into continuous measurement and discontinuous measurement. Each method serves different clinical purposes and offers unique advantages and limitations.
Continuous measurement captures every instance of behavior, while discontinuous measurement samples behavior during selected intervals. Research suggests that continuous methods are generally preferred because they provide a more accurate measure of target behavior. However, the method choice depends on practicality, behavior intensity, and clinical priorities.
Overall, a practitioner will apply:
- Continuous measurement when precision is required for treatment decisions.
- Discontinuous methods when continuous measurement is impractical and limitations are understood.
Continuous Measurement Methods
Continuous measurement records every occurrence of a behavior during an observation period. These methods are ideal when behaviors are discrete, countable, or when precision is essential for decision making.
Continuous methods include:
- Frequency / Event
- Rate
- Duration
- Latency
- Interresponse Time (IRT)
- Trial-by-Trial / Per Opportunity
Frequency / Event Recording
Frequency, or sometimes called event recording, measures the total number of times a behavior occurs within a specified observation period. In ABA therapy, frequency data provides a clear picture of how often a behavior occurs, making it ideal for skill acquisition and behavior reduction programs.
Examples:
- Counting how many times a child raises their hand during a session.
- Tracking the number of tantrums during a school day.
Benefits:
- Simple and intuitive to collect.
- Highly sensitive to changes in behavior.
- Ideal for discrete behaviors with clear start and end points.
Limitations:
- Not useful for behaviors that occur for long durations.
- Raw counts can be misleading when session lengths vary.
Software insight:
Digital tools like Office Puzzle allow therapists to record events in real time, reducing reliance on paper tallies and minimizing missed responses during busy sessions.
Rate Recording
Rate recording standardizes frequency by dividing the number of responses by time, resulting in a measure such as responses per minute or per hour. Rate data supports aligned comparisons across sessions, staff, and ABA environments. It is often preferred to inform clinical decisions when observation lengths vary.
Examples:
- A client blurts out 20 times during a 10 minute session, for a rate of 2 blurts per minute.
- A student raises their hand 6 times to ask a question in a 60 minute period.
Benefits:
- Allows accurate comparison across sessions of different lengths.
- More precise than frequency alone.
- Useful for tracking fluency and response intensity.
Limitations:
- Requires accurate session timing.
- More complex than simple frequency counts.
Software insight:
ABA software can automatically calculate rates from recorded frequency and session duration, eliminating manual math and improving data reliability.
Duration Recording
Duration recording measures how long a behavior lasts, from start to end. ABA clinicians use duration data to evaluate meaningful improvements that frequency alone cannot capture, such as shorter episodes of distress or longer engagement periods.
Examples:
- Measuring time spent engaged in independent work.
- Recording how long a client remains on task during instruction.
Benefits:
- Captures severity and impact of behaviors.
- Useful for endurance-based goals and emotional regulation targets.
Limitations:
- Requires continuous observation.
- Less useful for brief or rapid behaviors.
Software insight:
Built-in timers and automated duration tracking offered by ABA solutions such as Office Puzzle support consistent measurement across staff while reducing human error.
Latency Recording
Latency recording measures the time between a prompt or instruction and the initiation of a behavior. In ABA therapy, this data highlights improvements in independence and responsiveness, even when frequency of responding remains stable.
Examples:
- Time it takes a client to begin a task after being instructed.
- Measuring delay before responding to a direct question.
Benefits:
- Useful for addressing compliance and task initiation.
- Sensitive to motivation and prompt dependency.
Limitations:
- Requires precise timing.
- Not suitable for spontaneous behaviors.
Software insight
Digital latency tracking in systems like Office Puzzle allows clinicians to compare latency trends across sessions without manual stopwatch tracking.
Interresponse Time (IRT)
IRT measures the time between consecutive occurrences of the same behavior. IRT data is especially valuable for targeting fluency, self regulation, and behavior spacing goals in ABA therapy.
Examples:
- Tracking the time between completing and beginning math problems.
- Measuring spacing between tantrums in a session.
Benefits:
- Useful for shaping response patterns.
- Helps increase or decrease pacing of behaviors.
Limitations:
- Complex to track manually.
- Requires sustained attention from the observer.
Software insight:
Automated timestamps in ABA platforms calculate IRT without adding cognitive load to therapists, enabling deeper analysis with less effort.
Trial-by-Trial / Per Opportunity Recording
Trial-by-trial, or per opportunity recording, documents a client’s response following every instructional opportunity. Practitioners typically record responses as correct/incorrect or independent/prompted. In ABA practices this method is essential for monitoring learning progress, mastery criteria, and instructional effectiveness in structured programs.
Examples:
- Recording correct responses during discrete trial training (DTT).
- Tracking independent vs prompted responses in skill acquisition programs.
Benefits:
- Clear, objective data.
- Ideal for structured teaching and skill development.
- Easy to summarize as percentages.
Limitations:
- Limited to situations with clearly defined opportunities.
- Less informative for free operant, or natural behaviors.
Software insight:
Digital trial-by-trial data collection simplifies scoring, automatically calculates percentages, and supports consistent instructional decision making.
Continuous Measurement Summary
Continuous measurement provides the clearest behavioral picture and is considered best practice when feasible, particularly for treatment planning and progress monitoring.
Best use cases:
- Discrete behaviors.
- Skill acquisition programs.
- High risk or intensive intervention targets.
Benefits:
- Most accurate and sensitive data available.
- Supports ethical, data based treatment decisions.
Limitations:
- Time intensive.
- Can contribute to staff fatigue if done manually.
Software insight:
By consolidating multiple continuous data types into a single interface with automated summaries, modern software solutions help practices maintain precision while reducing administrative burden and burnout.
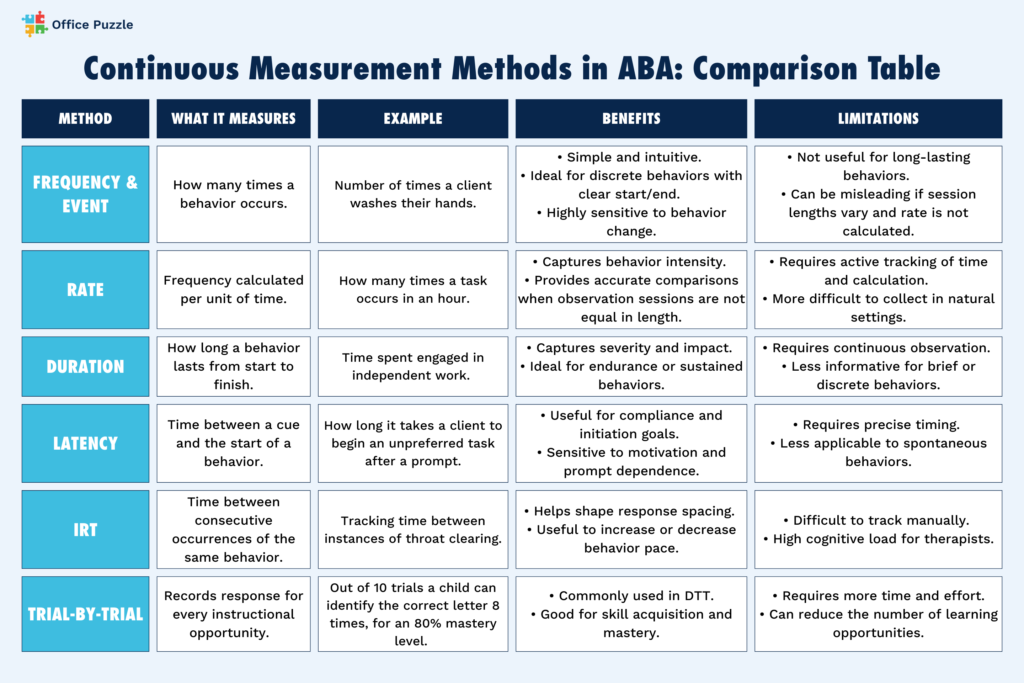
Continuous Measurement Methods in ABA: Comparison Table
Discontinuous Measurement Methods
Discontinuous measurement involves sampling behavior, rather than recording every occurrence. It includes interval recording and time sampling, where observations are broken into intervals to estimate occurrences or behavior is recorded during specific samples of a session. These methods are useful when continuous measurement is impractical due to staffing, setting, or behavior frequency.
The main types of discontinuous measurement are:
- Whole Interval Recording (WIR)
- Partial Interval Recording (PIR)
- Momentary Time Sampling (MTS)
- Planned Activity Check (PLACHECK)
Research finds that intervals of 3 min or less produced the greatest correspondence, and that MTS outperforms interval recording overall.
Whole Interval Recording (WIR)
WIR measures whether a behavior occurs for the entire duration of a predefined interval. It is best suited for goals that require maintaining behavior over time, such as remaining in a seat during instruction time.
Examples:
- Recording whether a client remains seated for a full 5-minute interval.
- Tracking sustained engagement during independent work periods.
Benefits:
- Encourages continuous, sustained behavior.
- Simple scoring, often marked as a “yes” or “no” per interval.
- Useful for endurance based goals.
Limitations:
- Can underestimate behavior.
- Does not capture partial occurrences within the interval.
Software insight:
Digital interval timers and automated prompts in platforms like Office Puzzle help staff maintain consistent intervals and reduce missed observations across sessions.
Partial Interval Recording (PIR)
PIR measures whether a behavior occurs at any point during the interval, even if it occurs briefly. This method is particularly helpful in ABA therapy when the goal is to reduce problem behavior, as it ensures brief instances are recorded.
Examples:
- Recording instances of yelling during a 10 minute observation period.
- Tracking occurrences of hitting in a classroom.
Benefits:
- Captures brief or repetitive behaviors.
- Easier to implement in fast paced settings.
- Useful for behavior reduction programs..
Limitations:
- Systematically overestimates behavior.
- Does not reflect frequency or duration.
Software insight:
With digital checkboxes and time-stamped intervals, software can simplify partial interval scoring while maintaining accurate session records.
Momentary Time Sampling (MTS)
MTS records whether a behavior is occurring at the exact moment the interval ends. This method is best for classroom and group settings where continuous observation is unrealistic but trend data is still valuable.
Examples:
- Observing whether a student is on task at the end of each 30-second interval.
- Measuring engagement during group instruction.
Benefits:
- Less labor intensive than other interval methods.
- Feasible for observing groups.
- Reduces observer fatigue.
Limitations:
- May miss behaviors occurring between intervals.
- Less sensitive to rapid behavior changes.
Software insight:
Automated alerts and prompts help observers collect data at the designated moments.
Planned Activity Check (PLACHECK)
PLACHECK is a type of momentary time sampling that measures whether a planned activity or expectation is occurring at specific moments. In ABA therapy, it is often used to evaluate implementation quality, classroom management strategies, and environmental arrangements.
Examples:
- Checking if students are engaged in assigned seatwork.
- Verifying whether a group is following outlined instructions during work time.
Benefits:
- Efficient for group and system monitoring.
- Supports treatment integrity and program fidelity.
- Minimal disruption to instruction.
Limitations:
- Does not capture individual performance details.
- Not suitable for measuring discrete behaviors.
Software insight
Digital PLACHECK tools within systems like Office Puzzle allow supervisors to quickly document program implementation across multiple environments and staff.
Discontinuous Measurement Summary
Discontinuous measurement samples behavior at specific moments or intervals rather than recording continuously. While discontinuous methods sacrifice precision, they play a critical role in maintaining consistent data collection when continuous measurement is not feasible.
Best use cases:
- Group or classroom settings.
- Long observation periods.
- Situations with limited staffing.
Benefits:
- Practical and time efficient.
- Reduces data collection burden.
Limitations:
- Less precise than continuous measurement.
- May overestimate or underestimate true behavior levels.
Software insight:
By standardizing intervals, prompting observers, and generating summaries automatically, a unified software solution helps ensure discontinuous data remains reliable and clinically useful.
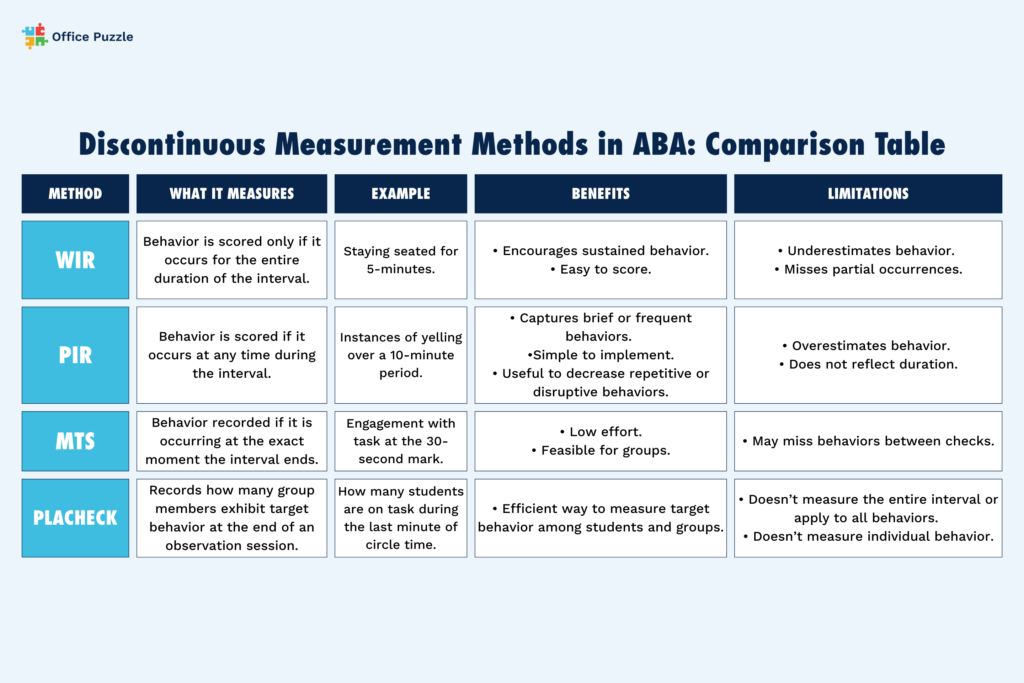
Discontinuous Measurement Methods Comparison Table
Other ABA Therapy Data Collection Techniques
ABC Data (Antecedent-Behavior-Consequence)
ABC data documents what happens before a behavior (antecedent), the behavior itself, and what occurs after the behavior (consequence). It identifies environmental variables that contribute to behavior and is a cornerstone of functional behavior assessment (FBA) for challenging behaviors.
Example:
A therapist records that a client is given a puzzle (antecedent), engages in throwing the puzzle pieces (behavior), and the puzzle is removed (consequence).
Scatterplot Analysis
Scatterplots map behavior patterns across times of day or settings to help identify patterns. The visualization helps clinicians determine trends and environmental correlations that may not be obvious through individual session data alone.
Example:
Instances of hitting are plotted across the school day and higher rates are noticed during early morning instruction times.
Permanent Product Recording
Measures outcomes of behavior rather than the behavior itself by focusing on tangible results. This method is practical when direct observation is difficult and allows for objective measurement after the behavior has occurred.
Example:
Tallying the number of independently completed math problems at the end of a working session.
Rating Scales and Checklists
Used for indirect measurement and caregiver or teacher input to estimate behavior frequency, severity, or skill performance.
Rating scales and checklists can provide broader contextual insight across settings and inform assessment, but should not replace direct observational data.
Example:
A teacher completes a behavior rating scale assessing attention and emotional regulation across the week.
Task Analysis
Breaks complex skills into smaller steps that can be individually measured to track acquisition and mastery. Task analysis supports skill acquisition programs by helping clinicians track progress and prompt levels for each step.
Example:
Simplify handwashing into the following steps: turn on water, apply soap, scrub, rinse, and dry hands.
Scatterplot and Rating Scale Combined
Combines objective scatterplot data patterns with subjective rating scale information to enhance clinical insight. This method can provide a more complete picture of behavior patterns and perceived impact across environments when analyzed carefully.
Example:
A clinician reviews a scatterplot showing increased problem behavior in the evenings alongside caregiver ratings indicating high family stress during that time.
Choosing the Right Data Collection Method
Selecting the best data collection method is a critical clinical decision. The goal is to gather accurate, meaningful data while balancing feasibility, staff capacity, and treatment objectives.
Selecting the right method depends on:
- Behavior type
- Environment
- Staff availability
- Clinical goals
Behavior Type
Discrete behaviors
Discrete behaviors have a clear beginning and end and occur as separate events.
Recommended measurement methods:
- Frequency / event recording & rate: when behavior occurs repeatedly across a session.
- Trial-by-trial (per opportunity) recording: when behavior follows a clear prompt or opportunity.
- Interresponse time (IRT) : when spacing between responses is clinically meaningful.
Continuous or extended behaviors
These behaviors occur over time or lack clear boundaries.
Recommended measurement methods:
- Duration recording: when severity or persistence matters.
- Whole interval recording: when building sustained engagement.
- Momentary time sampling: when continuous tracking is impractical
Environment: Clinic, Home, or School
The setting and goals determine the type of measurement that is best suited for your client.
Clinic-based settings
Are typically controlled environments with fewer distractions making it easier to apply continuous methods.
Home-based settings
Home settings often have variable routines that can include environmental distractions, and measurement requires family involvement. Monitoring duration for routines like homework or bedtime can be fitting for home settings. Partial interval or MTS can be applicable as long as caregivers have a clear understanding of the method.
School or group settings
Considerations include multiple students, limited attention of staff, and competing instructional demands. Discontinuous methods and a focus on trend data rather than exact counts can reduce observer burden. Recommended methods include MTS, partial or whole interval recording, and PLACHECK.
Staff Availability and Training Level
Measurement must be sustainable across all team members and account for the size of your staff and their training expertise.
High staff availability and training
When staffing and training are abundant, it allows for continuous measurement and more precise methods.
Limited staff availability or high caseloads
In this scenario, an ABA practice has a higher likelihood of missed or inaccurate data and a higher likelihood of burnout. Prioritize data consistency with simpler collection methods.
Clinical Goals of Intervention
The purpose of the data should guide measurement selection. Consider skill acquisition goals and keep a focus on learning, accuracy, and independence.
The best measurement method will:
- Accurately reflect the behavior
- Be implemented consistently
- Directly inform treatment decisions
When in doubt, clinicians should revisit the BACB Ethics Code requirement to use measurement systems that are appropriate to the behavior and feasible in the environment.
Best Practices for Collecting Reliable Data
Reliable data allows clinicians to make sound treatment decisions and ensure that interventions genuinely benefit the client.
- Use clear operational definitions
- Implement consistent staff training
- Conduct inter-observer agreement (IOA) checks
- Review data frequently
- Use visual analysis to guide decisions
It’s important to remember that measurement should support care, not overwhelm the people delivering or receiving it.
Use Clear, Operational Definitions
Operational definitions are a core requirement of behavior measurement and are emphasized throughout ABA research methodology and the BACB Ethics Code. These standardized definitions create consistency for practitioners by ensuring that the same behavior is measured in the same way.
Best practices:
- Define behaviors in observable and measurable terms.
- Use specific, descriptive language: instead of “upset,” use “screaming.”
- Include examples and non-examples when possible.
- Specify onset and offset criteria for timing-based measures.
Train Staff Consistently
Studies show that observer training and feedback improve data accuracy and quality, especially in applied settings.
Best practices:
- Provide initial training on each data collection method.
- Use modeling, practice opportunities, and feedback.
- Offer training when methods change or new staff join.
- Implement fidelity checks to monitor for drift.
Conduct Inter-Observer Agreement (IOA) Checks
The BACB Ethics Code emphasizes using measurement systems capable of producing accurate and reliable data, and IOA is essential to meeting that standard.
Best practices:
- Conduct IOA regularly, not just during supervision.
- Aim for at least 20–30% of sessions, across different conditions.
- Use appropriate IOA methods for the data type.
- Investigate and retrain if agreement falls below acceptable levels.
Review Data Frequently
Data only improves care if it is actively used to inform treatment. ABA outcomes are strongest when treatment decisions are made frequently and proactively, rather than waiting for long review cycles.
Best practices:
- Review data at least weekly or more often for intensive cases.
- Look for trends, level changes, and variability.
Compare data to treatment goals and mastery criteria. - Adjust interventions when data indicate stagnation or regression.
Use Visual Analysis to Guide Decisions
Visual analysis is a cornerstone of ABA that supports transparent, evidence-based treatment decisions. It can reveal changes over time that are missed in statistics alone, and makes data more accessible to teams and clients.
Best practices:
- Graph data consistently and clearly
- Examine level, trend, variability, and immediacy of change
- Compare baseline and intervention phases
- Avoid reliance on averages alone
Using Data to Inform Interventions
In ABA therapy, data is used to continuously evaluate necessary and effective treatment. Access to real time and dependable information allows clinicians to respond quickly and ethically as a client’s needs change.
Below are some of the most practical applications for data-informed interventions in ABA settings.
Skill progression
Data guides clinical decisions like when to advance, maintain, or revisit skills.
Best practices:
- Use clearly defined, measurable mastery criteria.
- Review trends over time rather than relying on single-session performance.
- Advance skills only when data shows stable, independent responding.
Prompt fading
Reliable data helps to determine the timing and approach to prompt fading in ABA therapy.
Best practices:
- Track prompt level such as full physical, partial, gestural, or independent.
- Monitor latency for the time between cue and response and independence trends.
- Adjust prompts when data shows prompt dependency.
Reinforcement adjustments
Reinforcement effectiveness in ABA therapy changes over time, and data indicates when adjustments are needed.
Best practices:
- Track declining response rates despite consistent reinforcement.
- Monitor changes in engagement or motivation and consider shifts such as extrinsic to natural reinforcement.
- Note differences in performance across settings or staff and adjust approach.
- Apply data insights to modify reinforcement schedules by decreasing/thinning or increasing/densifying.
Program modifications
When data shows limited progress, ABA practitioners must make timely program modifications to ensure client success.
Best practices:
- Address flat or declining trends with program modifications such as changing instructional procedures.
- Monitor for high variability without improvement and adjust antecedents or task difficulty.
- Track lack of generalization or maintenance and reassess function or skill prerequisites.
The Role of Software in ABA Data Collection
As ABA practices grow and face increasing care demands, software has become essential to maintaining ethical and clinically useful data systems. Modern ABA software is designed to support the entire clinical workflow, from individual session data, to compliance, reporting, and managing operations. And, when clinical and administrative systems are unified in one platform, practices are better positioned to deliver consistent, quality care while reducing strain on staff.
Integrating effective software into your ABA practice results in the following benefits.
Streamlined Data Collection and Integrity
Digital data collection improves consistency by standardizing how behaviors, prompts, and outcomes are recorded. Features like programmed definitions, required fields, and real-time validation help reduce variability across staff and settings, strengthening treatment integrity.
Timely, Actionable Analysis
Software allows data to be graphed automatically and reviewed immediately, supporting visual analysis and faster clinical decision making. This reduces delays between data collection and treatment adjustments, enabling practitioners to implement insights in the moment and over time.
Reduced Paperwork and Administrative Burden
Software can consolidate session notes, treatment plans, progress reports, authorizations, and billing documentation in one system. The reduction in manual documentation helps minimize reiterative processes and duplicate forms which can alleviate overall staff burden. And, with the right system in place, clinicians can spend more time delivering care rather than managing paperwork.
Minimizes Human Error
Automation in software platforms reduces errors associated with data entry and transcription. Features like time stamps, locked notes, and audit trails support accuracy and compliance with payer and regulatory requirements.
Supports Interdisciplinary and Multi-Setting Care
Software platforms, especially those with unified systems, allow data to travel with clients across providers, locations, and services. This results in improved collaboration and treatment consistency.
Connecting Clinical Data to Business Operations
When clinical data, scheduling, authorizations, and billing are integrated, practices gain clearer insight into service delivery and outcomes. This alignment supports practice growth without compromising the quality of care.
How Office Puzzle Streamlines Data Collection Across Your Entire ABA Practice
Clinical software should support care, not overwhelm the people delivering it. Office Puzzle was built for a BCBA who needed an all-in-one ABA solution, and has grown to help thousands of others to streamline their workflow so they can focus on care.
Office Puzzle’s unified platform integrates data collection with scheduling, billing, notes and reporting to reduce administrative burden, promote scalability, and enhance clinical quality.
Office Puzzle streamlines ABA data collection with:
- A clean, intuitive interface that lowers training time and makes daily navigation easier.
- Integrated clinical & administrative tools: no switching between systems or duplicating work.
- Automated workflows for less manual follow up and fewer missed tasks.
- Built-in compliance tools that reduce audit anxiety and rework.
- Flexible workflows & templates: practices can align documentation and data collection with their clinical model instead of changing how they work.
- Mobile access: collect data and complete notes across multiple settings without delays.
Ready to experience the difference for yourself? Try Office Puzzle free for 30 days, no payment information collected, no sales pitch or demo. Simply fill out our trial request form and you’re in. Get started now.
Frequently Asked Questions
What is the difference between continuous and discontinuous measurement in ABA?
Continuous measurement records every instance of behavior, while discontinuous measurement samples behavior during intervals.
When should I use frequency vs rate recording?
Use frequency when session lengths are consistent; use rate when comparing across different session durations.
What is ABC data collection and why is it important?
ABC data helps identify behavior function by analyzing antecedents and consequences, informing effective intervention design.
How does software like Office Puzzle simplify data collection?
It automates calculations, standardizes data entry, reduces errors, and integrates clinical and administrative workflows.
Why do I need inter-observer agreement (IOA)?
IOA ensures data reliability and confirms that behavior definitions and measurement systems are applied consistently.
References
- Autism Speaks. Autism prevalence rises to 1 in 31 children in the U.S. https://www.autismspeaks.org/science-news/autism-prevalence-rises-1-31-children-us
- Autism Speaks. Behavior definitions. https://docs.autismspeaks.org/behaviors-overview/definitions
- Behavior Analyst Certification Board. (2025). Lightcast workforce analysis report 2025. https://www.bacb.com/wp-content/uploads/2025/02/Lightcast2025_250204-a.pdf
- Behavior Analyst Certification Board. (2024). Ethics code for behavior analysts. https://www.bacb.com/wp-content/uploads/2022/01/Ethics-Code-for-Behavior-Analysts-240830-a.pdf
- Cooper, J. O., Heron, T. E., & Heward, W. L. (2020). Applied behavior analysis (3rd ed.). Pearson.
(Original work published 2007) - Gast, D. L., & Ledford, J. R. (Eds.). (2014). Single-case research methodology: Applications in special education and behavioral sciences (2nd ed.). Routledge.
- Hanley, G. P., Iwata, B. A., & McCord, B. E. (2003). Functional analysis of problem behavior: A review. Journal of Applied Behavior Analysis, 36(2), 147–185. https://pmc.ncbi.nlm.nih.gov/articles/PMC2521856/
- Ledford, J. R., & Gast, D. L. (2018). Measuring behavior in single-case research. Behavior Analysis in Practice, 11(3), 236–246. https://pmc.ncbi.nlm.nih.gov/articles/PMC5172380/
- Mudford, O. C., Taylor, S. A., & Martin, N. T. (2009). Continuous recording methods. Behavior Modification, 33(4), 546–575. https://pmc.ncbi.nlm.nih.gov/articles/PMC3592492/
- Petursdottir, A. I., & Carr, J. E. (2011). A review of recommendations for calculating interobserver agreement. Journal of Applied Behavior Analysis, 44(2), 377–390. https://pmc.ncbi.nlm.nih.gov/articles/PMC2521856/
- Shadish, W. R., Cook, T. D., & Campbell, D. T. (2002). Experimental and quasi-experimental designs for generalized causal inference. Houghton Mifflin.
- Stewart, K. K., McGee, G. G., & Fryling, M. J. (2020). Practical considerations for data collection in applied behavior analysis. Behavior Analysis in Practice, 13(4), 863–876. https://pmc.ncbi.nlm.nih.gov/articles/PMC7314895/